India’s vast rural expanse, home to more than two-thirds of the nation’s population, faces formidable challenges in accessing quality healthcare. Limited infrastructure, a shortage of qualified medical professionals, and geographic barriers create significant disparities between urban and rural healthcare delivery. Digital health solutions are emerging as a potent force in revolutionizing this landscape, promising to deliver equitable and accessible healthcare to India’s underserved rural communities.

Key Pillars of Digital Health Intervention
- Telemedicine and Remote Consultations: At the forefront of digital health, telemedicine platforms are bridging the gap between patients in remote villages and specialists residing in faraway urban centres. These platforms facilitate real-time video consultations, allowing rural patients to receive diagnoses, treatment plans, and follow-up care without the need for arduous journeys to cities. This significantly reduces travel costs, time, and the burden on rural families.
- Electronic Health Records (EHRs): Digitizing patient records is instrumental in improving care coordination and reducing medical errors. With EHRs, healthcare providers across different locations can access a patient’s medical history, ensuring continuity of care and informed decision-making. Digital records also streamline the referral process and aid in disease surveillance and outbreak management.

- Mobile Health (mHealth) Applications: The proliferation of smartphones and internet connectivity has made mHealth apps a valuable tool for rural communities. These apps provide health education, preventive care information, medication reminders, and symptom checkers, empowering individuals to take charge of their health. In particular, pregnancy tracking and maternal health apps are proving to be lifelines in remote areas.
- Remote Patient Monitoring (RPM): RPM technology allows healthcare providers to track vital signs, such as blood pressure and blood sugar, of patients with chronic diseases from afar. This proactive monitoring enables early interventions, facilitates timely adjustments to treatment plans, and reduces the risk of expensive hospitalizations.
- Point-of-Care Diagnostics: Portable diagnostic devices connected to smartphones or tablets are bringing laboratory-quality testing to remote corners of India. These devices can perform tests for infectious diseases, anaemia, and other conditions, leading to rapid diagnoses and faster treatment initiation, which is crucial in resource-limited settings.
Benefits of Digital Health for Rural India
- Improved Access to Care: Digital health transcends geographical barriers and overcomes the lack of specialists in rural areas. Patients can access essential medical services without the hardship and expense of traveling long distances.
- Enhanced Quality of Care: EHRs and telemedicine consultations with specialists support rural healthcare providers in delivering higher quality care, leading to improved patient outcomes.

- Cost Reduction: Digital health solutions reduce patient travel costs, minimize unnecessary hospitalizations, and improve efficiency in healthcare delivery, contributing to overall cost savings.
- Preventive Care and Empowerment: mHealth apps and educational resources empower rural communities to adopt healthier lifestyles, practice preventive care, and make informed decisions about their health.
Challenges and Considerations
While the transformative potential of digital health is undeniable, its widespread adoption in rural India faces hurdles:
- Digital Literacy & Adoption: Limited digital literacy and technological skills among some rural populations can hinder the uptake of digital health solutions.
- Infrastructure: Unreliable internet connectivity and electricity supply in certain areas pose challenges for telemedicine and other digital health interventions.
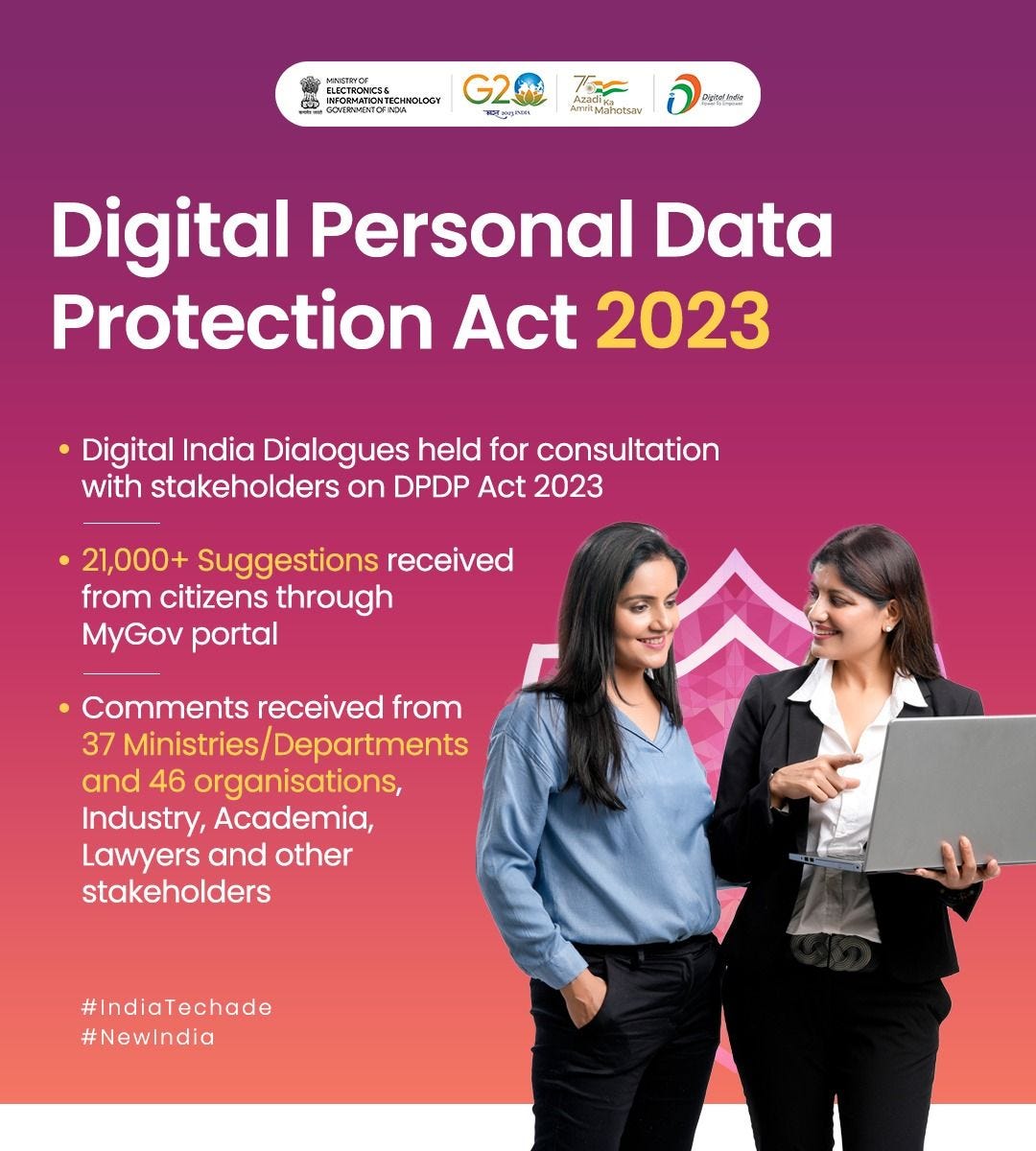
- Data Security and Privacy: Robust measures are needed to ensure the security and privacy of sensitive patient data in the digital realm. In this regard Government of India passed The Digital Personal Data Protection Act (DPDPA) in August 2023. DPDPA assigns restrictions and obligations to organizations that process personal data including sensitive patient data.
The Way Forward
To fully realize the benefits of digital health in improving rural healthcare in India, collaborative efforts among government, healthcare providers, technology companies, and communities are vital. Key measures include:
- Investing in Digital Infrastructure: Expanding broadband connectivity and ensuring reliable electricity supply in rural areas.
- Digital Literacy Campaigns: Educating rural communities on the use of digital tools, promoting their adoption.

- Government Initiatives: Continued support and favourable policies, including the Ayushman Bharat Digital Mission by National Health Authority (NHA), are key to scaling digital health initiatives. The Ayushman Bharat Digital Mission has the potential to transform the landscape of rural healthcare in India. Its focus on interoperability, inclusivity, and patient empowerment directly addresses the unique challenges of healthcare delivery in these regions.
- Partnerships and Capacity Building: Training rural healthcare workers in digital health technologies and fostering collaboration between healthcare providers and technology innovators.
Digital health holds the key to bridging the healthcare divide between rural and urban India. Its strategic implementation offers an unprecedented opportunity to deliver affordable, accessible, and high-quality healthcare to the doorstep of those who need it the most.