Many people
have heard a lot about the blockchain in frames of a cryptocurrency called
Bitcoin; however, it can have a much wider use than a simple payment method,
including various industries. So, how does blockchain actually work in the
healthcare industry?
Health Care and Interoperability
Interoperability is a huge problem in the healthcare industry. In fact, improved healthcare interoperability is been a top priority for providers, policymakers, and patients for quite some time now.
So what are the two major areas when it comes to ineffective interoperability?
- The trouble of identifying patients
- Information blocking
The trouble of Identifying Patients
One of the most surprising things that we learned while researching for this guide. Apparently, there is still no universally recognized patient identifier. This despite the fact that organizations like CHIME and HIMSS have been pushing for its development for almost two decades.
This is truly shocking when you consider the fact that a unique patient identifier will be able to easily solve the problem of mismatched patient EHRs (Electronic health record) which has in the past led to several errors in patient care and increased the likelihood of patient harm.
This problem has been well expressed by the Director of Center for Biomedical Informatics (CBMI), Shaun Grannis.
“Matching the correct individual to his or her health data is critical to their medical care,” he says. “Statistics show that up to one in five patient records are not accurately matched even within the same health care system. As many as half of the patient records are mismatched when data is transferred between healthcare systems.”
So, how can the blockchain potentially solve this problem? Well, let’s look into it in a bit. Before we do so let’s look at the second problem that we have here.
Information Blocking
Despite being deemed an illegal practice, information blocking has been a problem in the healthcare industry. What do we mean by information blocking?
In the healthcare industry, information blocking is described as the result of “an unreasonable constraint imposed on the exchange of patient data or electronic health information.” According to the U.S. Office of the National Coordinator for Health Information Technology, there are three criteria for identifying information blocking:
- There has been interference
- There has been knowledge
- There is no reason for the data to not be accessible.
It goes without saying that information blocking practices that involve unreasonable interference and awareness are a huge detriment to an efficient healthcare practice. Blocking can take place because of policies that prevent the sharing of information as well as practices that makes sharing extremely impractical.
The reason for this is pretty straightforward. Hospitals don’t want to lose out on patients and want to make it as difficult as possible for them to want to move on to another hospital.
In this digital age, this should have been a draconian practice, but various surveys and studies say otherwise.
- After surveying 60 HIE leaders, it was discovered that information blocking is extremely widespread and the various actions that have been taken to curb it are still extremely ineffective.
- 50% of respondents that have been studied by Adler-Milstein reportedly engaged with health IT companies by participating in information blocking. A quarter of these respondents also said that hospitals and health systems are guilty of this practice.
According to the researchers, information blocking can be curbed by one of the following methods:
- By increasing transparency so that each and every action that has been taken by the participants can be accounted for.
- There should be a strong financial incentive so that the participants will want to share information with each other.
- A collaborative relationship between health IT companies, hospitals, and HIEs could further curb information blocking.
Alright, so now we have acquainted ourselves with the interoperability issues that are eating up the healthcare industry from the inside. Now let’s see how the blockchain is going to help solve this issue.
Public and Private Blockchains
There are two specific kinds of blockchains out there:
- Public Blockchains
- Private Blockchains
Since both are blockchains, they provide a peer-to-peer network which offers a decentralized and immutable ecosystem which are synchronized via consensus protocols.
However, that’s where all the similarities end.
Public Chains
Public blockchains are the ones that we are most familiar with. Bitcoin, Ethereum etc. are all public blockchains and the reason why they are called so is pretty self-explanatory.
They are completely open ecosystems where anyone can take part in the ecosystem. The network also has an in-built incentive mechanism which rewards participants for taking part more thoroughly in the system.
So, that’s pretty awesome right, however, will the health care industry benefit from having a public blockchain? Well…not so much.
Firstly, as has been extremely well documented, the blocks in bitcoin and ethereum have a storage issue. Bitcoin has a little over 1mb of space per block which is simply not enough to run the kind of transactions and store the kind of data that healthcare institutes require.
Then we have the throughput problems which have also been pretty well-documented. Bitcoin can barely manage 7-8 transactions per second. The block confirmation time is 10 mins which just adds to the latency. Big healthcare institutes need to deal with huge blocks of transactions per day with near 0 latency. In fact, any sorts of latency can potentially be life-threatening
Public blockchains, especially the ones that follow the proof-of-work protocol like Bitcoin require an immense amount of computational power to solve hard puzzles. As such, it is really impractical for these institutes to spend so much money on consensus mechanisms.
Finally, public blockchains are open chains, which in itself is another detriment. Think about it, why should healthcare institutes try to interact with each other in a network where anyone can come in and become a part of it. Medical insitutes deal with highly-classified and sensitive data, why will they want anyone outside their circles to interact with it?
So, public chains are impractical for these purposes. However, there is one more kind of blockchain that is practical for healthcare institutes, and they are called private blockchains.
Private Chains
Private chains are..well…private.
Unlike public blockchains, these aren’t open to everyone. As a result, people who want to participate in the private chain must gain permission to be a part of this network. This is the reason why private chains are also called “permissioned blockchains.”
Because of this, there are restrictions to the kind of people who can actually take part in the consensus. Access for new participants could be given by the following:
- The existing participants who are taking part in the ecosystem.
- A regulated authority.
- A consortium.
Once an entity has joined the ecosystem, they can play a role in network maintenance. The Linux Foundation’s Hyperledger Fabric is an example of a permissioned blockchain framework implementation and one of the Hyperledger projects hosted by The Linux Foundation. It has been designed ground up to cater to these enterprise requirements.
These private chains have been specifically designed for enterprise needs and offer a lot of features like:
- Fast transactions
- Privacy
- High security
Ok, so we have one side of the equation, which is the private chain. However, there is one more piece of the puzzle that we must understand before we wrap our heads around how the medical industry will work on the blockchain.
Cryptographic Hash Functions
Hashing means taking an input string of any length and giving out an output of a fixed length. In the context of cryptocurrencies like Bitcoin, the transactions are taken as an input and run through a hashing algorithm (Bitcoin uses SHA-256) which gives an output of a fixed length.
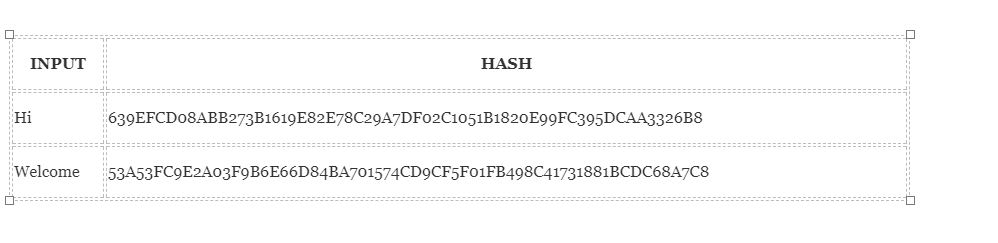
Let’s see how the hashing process works. We are going put in certain inputs. For this exercise, we are going to use the SHA-256 (Secure Hashing Algorithm 256).
There are quite a lot of properties that makes hash functions pretty darn useful. We have covered these earlier, however, let’s focus on a few of them for now.
Property 1: Deterministic
This means that no matter how many times you parse through a particular input through a hash function you will always get the same result. This is critical because if you get different hashes every single time it will be impossible to keep track of the input.
Property 2: Pre-Image Resistance
What pre-image resistance states is that given H(A) it is infeasible to determine A, where A is the input and H(A) is the output hash. Let’s take an example.
Here is a hash:
559AEAD08264D5795D3909718CDD05ABD49572E84FE55590EEF31A88A08FDFFD
Can you determine what was the input that generated this exact hash? You will have a hard time determining it. It won’t be impossible, it will just be extremely irritating and time-consuming.
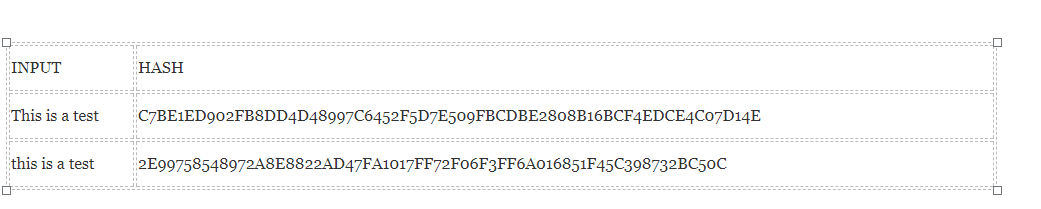
Property 3: Snowball Effect
This property states that even if you make a small change in your input, the changes that will be reflected in the hash will be huge. Let’s test it out using SHA-256:
You see that? Even though you just changed the case of the first alphabet of the input, look at how much that has affected the output hash.
Now let’s bring it all together and see how a permissioned blockchain can help end the interoperability problem in the healthcare industry.
Permissioned Healthcare Blockchain
Imagine a network on healthcare institutes where they don’t own a patient’s personal data. The data all belong in the blockchain. The patients are identified via their hash ID which will be their unique identifier. The hashing allows the ID to be unique and secures the privacy of the user (see Property #2 above).
The blockchain can also aid in the creation of a patient information sharing marketplace. This way, it will be possible to actually incentivize information sharing between the different institutes to prevent any kind of info blocking.
However, what if we still have some malicious actors who attempt to do information blocking or tampering?
In that case two of the blockchain’s most significant features will step up and handle this situation:
Firstly, the blockchain is a transparent medium. Anyone, who is part of the network, can look into the blockchain and look at how each transaction takes place and whether all the relevant information is getting passed through or not.
Secondly, we have anti-tampering.
If anyone tries to block the data then via the snowball effect, it will change the hash drastically. Now, remember, that the blocks in the blockchain are linked to one another via a hash pointer. Each block in the blockchain stores the hash of the data that is stored in the previous block. If the data inside any one of the blocks change, it sets up a chain reaction which could freeze up the whole blockchain. Since this is a theoretical impossibility, it is impossible to tamper with any data that is inside the blockchain.
Other Advantages of the Medical Healthcare Blockchain
So, now that we know how interoperability can be solved, what other amazing advantages can the blockchain bring to the medical healthcare institute?
- Since the blockchain is Immutable and traceable, patients can easily send records to anyone without the fear of data corruption or tampering.
- Similarly, a medical record that has been generated and added to the blockchain will be completely secure.
- The patient can have some control over how their medical data gets used and shared by the institutes. Any party which is looking to get the medical data about a patient could check with the blockchain to get the necessary permission.
- The patient can also be incentivized to for good behavior via a reward mechanism. Eg. they can get tokens for following a care plan or for staying healthy. Also, they can be rewarded by tokens for giving their data for clinical trials and research
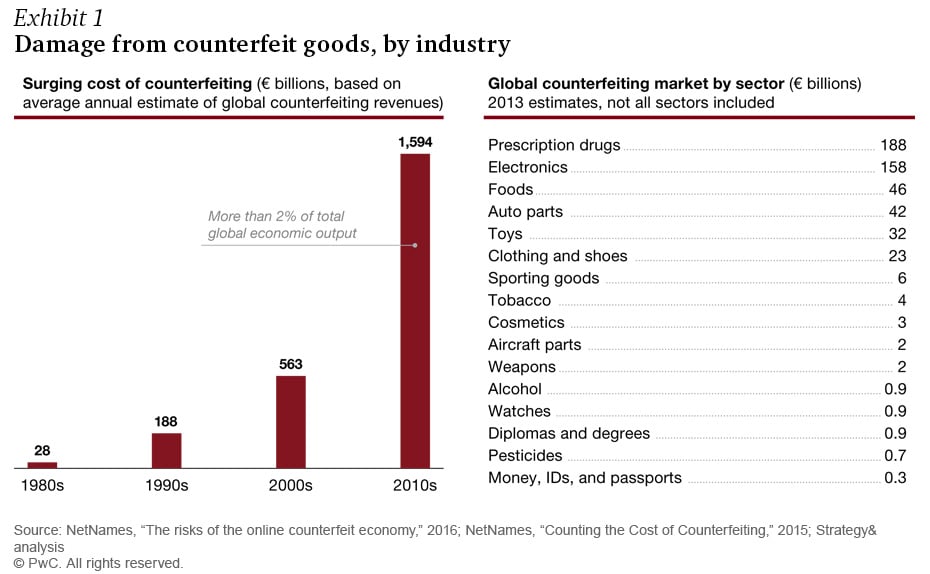
Pharma companies need to have an extremely secure supply chain because of the kind of product they carry. Pharma drugs are consistently stolen from the supply chain to be sold illegally to various consumers. Also, counterfeit drugs alone cost these companies, nearly $200 billion annually. A transparent blockchain will help these companies to enable close tracking of drugs to their point of origin and thus help eliminate falsified medication.
- Various medical institutes around the world conduct their own research and clinical trials on various new drugs and medications. A blockchain will help create a single global database to collect all this data and put them in one place.
Insurance fraud is a major problem that is affecting the healthcare industry. This happens when dishonest providers and patients submit false claims/information to receive payable benefits. To get an understanding of how serious this problem is, try to wrap your head around this: According to Boyd Insurance, Medicare fraud in the U.S. alone costs about $68 billion a year.
In fact, according to the charts, the top two kinds of healthcare frauds are healthcare related.
Jack Liu, CEO of ALLIVE, an intelligent healthcare ecosystem based on blockchain technology, believes that the blockchain is going to help solve this problem. According to him,
“A blockchain environment can eliminate a large portion of this fraud when providers and patients must enter their information and data to be verified, recorded and stored and health insurance companies must have access to that data.”
Since all the data will not be stored in a centralized infrastructure, it will be impossible to hack the system and get their hands on all of the data. This keeps the system leakage-free and it also helps secure the privacy of the patients.
The Detractors
Obviously, not everyone is on-board with the idea of basing the healthcare industry on the and around the blockchain technology. One of those detractors happens to be John Halamka, the Chief Information Officer of Beth Israel Deaconess Medical Center in Boston, a Harvard University teaching hospital. He has already worked on several production blockchain applications, so he is intimately familiar with how it works and its potential use-cases.
According to him,
“Blockchain is not meant for storage of large data sets. Blockchain is not an analytics platform. Blockchain has very slow transactional performance. However, as a tamperproof public ledger, blockchain is ideal for proof of work. Blockchain is highly resilient”.
Blockchain in HealthcareConclusion
So, there you have it. We have listed down the various advantages that the blockchain can potentially impart to the healthcare industry. Obviously, until we see a proper implementation of this partnership, this is all hearsay. What we can state for a fact, is that various other institutes and spaces have already started experimenting and working with the blockchain technology.
This space has no lack of money. In fact, consider the following statistics:
- The funding of digital health startups reached an all-time high in the first quarter of 2018
- Global annual health spending surpassed $7 trillion dollars in 2015
- By 2020, the global annual health spending is expected to have ballooned to over $8.734 trillion.
As such, they should be under no financial constraints to research new and exciting technologies. All signs are pointing towards a decentralized medical future. Let’s see why.
According to a report by BIS research, by 2025, the healthcare industry can save upto $100 billion per year by 2025 in data breach-related costs, IT costs, operations costs, support function and personnel costs, counterfeit-related frauds and insurance frauds if they incorporate the blockchain technology.
The report also states that the use of
“a global blockchain in the healthcare market is expected grow at a CAGR of 63.85% from 2018 to 2025, to reach a value of $5.61 billion by 2025. The use of blockchain for healthcare data exchange will contribute the largest market share throughout the forecast period, reaching a value of $1.89 billion by 2025, owing to the use of blockchain to solve the most widespread problem in healthcare information systems related to interoperability and non-standardization that has created data silos in the industry.”
According to the report and the way the blockchain is being adopted by various sectors, it definitely looks like the future of the healthcare industry is indeed decentralized. Let’s hope that the blockchain technology provides the horizontal innovation boost to this industry that it desperately needs.
Major portion of this article taken from